
Bariatric Surgeon Sydney
Dr John Jorgensen is one of Australia’s most experienced bariatric and Upper GI surgeons.
He has been in specialised surgical practice for more than three decades and is currently the Director of Bariatric Surgical Services at St George Private Hospital, Australia’s highest volume bariatric hospital.
Dr Jorgensen graduated from The University of New South Wales with honours, (MBBS) and obtained his Fellow in Royal Australian College of Surgeons (FRACS) in 1991.
He then commenced a Master of Surgery, Research degree in Laparoscopic Surgery, and further trained at the Pancreatic and Biliary Surgical Unit at The Royal Infirmary Glasgow, Scotland. In 2000 he had a twelve month sabbatical at the University Hospital in Lund, Sweden, focusing on bariatric surgery.
Since his return to practice in Sydney he has focused on providing multidisciplinary care for the severely obese.
Dr Jorgensen also specialises in Upper GI Surgical procedures such as hernia surgery, gallbladder surgery, reflux surgery and gastric and
oesophageal cancer.
Contact Our Team
ALL APPOINTMENTS: 02 9553 7288
Dr Jorgensen consults at Level 5, Suite 19
St George Private Hospital 1 South Street KOGARAH NSW 2217
%
The number of overweight or obese Australians by 2025
International health organisations that now endorse bariatric surgery as standard treatment for diabetes
St George Private is Australia's No 1 bariatric hospital by volume
Dr John Jorgensen is one of Australia’s most experienced bariatric and Upper GI surgeons.
He has been in specialized surgical practice for more than three decades and is currently the Director of Bariatric Surgical Services at St George Private Hospital, Australia’s highest volume bariatric hospital.
Dr Jorgensen graduated from The University of New South Wales with honours, (MBBS) and obtained his Fellow in Royal Australian College of Surgeons (FRACS) in 1991.
He then commenced a Master of Surgery, Research degree in Laparoscopic Surgery, and further trained at the Pancreatic and Biliary Surgical Unit at The Royal Infirmary Glasgow, Scotland. In 2000 he had a twelve month sabbatical at the University Hospital in Lund, Sweden, focusing on bariatric surgery.
Since his return to practice in Sydney he has focused on providing multidisciplinary care for the severely obese.
Dr Jorgensen also specialises in Upper GI Surgical procedures such as hernia surgery, gallbladder surgery, reflux surgery, and gastric and oesophageal cancer.
Your Bariatric Surgery Journey

Let your journey start here
Our Bariatric Program has been carefully designed to ensure your peace of mind and comfort with ongoing care well beyond the surgery alone.
View More
During your first consultation you will be first seen by our nurse practitioner Silvia, who will take an extensive clinical history.
During your first consult Dr Jorgensen and his nurse will discuss your blood test results and any co-existing health conditions you may have.
As there is no one-size-fits-all approach for bariatric surgery, Dr Jorgensen will weigh up the pros and cons of each bariatric procedure, ensuring your operation is customised to your health, personality and lifestyle.
You will then have another follow up with the dietitian before surgery.

Having your surgery
Prepare for surgery over 2 – 4 weeks with your VLCD as recommended.
Have your surgery at a private hospital. Full Multidisiplinary care.
View More
On the day of your surgery, when you wake up there will be a “patient controlled analgesic” (PCA) pump connected to your IV drip.
This works very well for pain control and is usually removed the next day and oral analgesia is given.
Most people can sit up, mobilize and move their legs a few hours after the operation, and this is also highly encouraged.
The day of surgery you will start a “free fluid” diet this may include yoghurt, custard, milk, soup and diet cordial.
You will probably be discharged on day two post op, and will be required to take medications with you when you leave as prescribed.

After your surgery long term
You will be asked to follow the CSIRO Low-Carb Diet and lifestyle solution Book, a scientifically proven lifestyle guide for losing weight and improving health.
View More
You will also be reviewed by our nurse at 3 weeks. If you have any surgical issues Dr Jorgensen will see you. You will then need to come back to the rooms for reviews at 3, 6, 9, 12, 18, and 24 months post-surgery.
All bariatric-related consults post-surgery with either Dr Jorgensen, his dietitian or his nurse will be cost-free to the patient for two years with active referral.
These consults are unlimited and included in Dr Jorgensen’s one-off surgical service fee.
Keeping regular appointments with Dr Jorgensen and his team – either face to face or online or via phone – will help you stay on track.

Nutrition
-Will I have to go on a diet before I have surgery?
-Will I have to be on a diet after the surgery?
Learn More
Pre-Op Very Low Energy Diet (VLED)
Following a strict pre-operative diet is very essential for patients undergoing weight-loss surgery in order to decrease the size of the liver and facilitate minimally invasive (laparoscopic) surgery safely, which is associated with less post-operative pain and faster recovery.
If you are diabetic, your diabetic medication will need to be adjusted by your diabetes nurse educator, GP or endocrinologist.
What is the pre-op diet stage?
• You will begin the pre-op diet stage about 2-4 weeks before surgery. Your bariatric
surgery healthcare team will tell you when you need to start this diet.
• This stage involves following a Very Low Energy Diet (VLED). VLED may also be called
a VLCD (very low-calorie diet).
• The most common VLED product recommended is Formulite and Optifast other products can be considered so discuss with our dietitian.
Your bariatric surgery healthcare team may recommend an alternative product. This will be based on any pre-existing medical conditions you may have.
• Strictly follow the instructions for taking your VLED . If you do not follow the pre-op diet
stage correctly, the size of your liver may not reduce, and your surgery could be cancelled.
How do they work?
• VLED meal replacement products are very low in carbohydrates, which will cause your
body to go into mild ketosis.
• During ketosis, the body switches from using carbohydrates as the main source of
energy, to using your body fat.
• Ketosis will assist to reduce the size of your liver. This will allow your surgeon to better
access your stomach.
• This means it is extremely important to follow the plan. Do not include any extra
carbohydrates (e.g. breads, grains, cereals, fruit, dairy foods like milk or yoghurt or
sugars) which can stop the ketosis process.
• A VLED meal replacement plan will assist with reducing your body weight and improving
your nutrition before surgery.
Common challenges.
During the first 3 days of this diet, you may experience some of the following symptoms:
• Fatigue
• Hunger
• Nausea
• Poor concentration
• Dizziness / light-headedness
• Headaches
• Diarrhoea
Ensure you continue to follow the VLED plan and drink plenty of fluids during this time.
After 3-4 days your body should adapt, and you should feel much better
Post-operative diet.
You will also need to follow a specific diet plan after bariatric surgery.
Immediately after the surgery, a special diet will allow your stomach to heal. Initially, the stomach does not contract very well, so you will consume liquids/purees only for the first 3 weeks. This means no solid food at all during the first 3 weeks post-op diet.
Three weeks after weight loss surgery.
You can start to eat soft and moist foods. We can help you make a bariatric diet food list for guidance, or just use the resource book given to you. You will be able to manage most food textures by 6 weeks after surgery. Some foods, such as chicken breast or well-done steak, often take longer to manage. Occasionally there may be a food that just never sits well in the stomach after surgery.
Keep in mind.
You will need to learn to eat slowly, chew food well, and get used to not finishing meals.
The following points are important to keep in mind:
Everyone progresses at different rates with what foods they can manage after surgery, the amount of food they can eat comfortably, and their rate of weight loss.
It can take some people weeks to get used to eating smaller amounts of food and not finishing meals. You will adjust though; it just takes some time and patience.
Here are a few things that you can try when eating out:
Only order small meals, entrees rather than main courses; share food with others at your table; ask to take leftovers home when eating out at restaurants and cafes.
After a gastric bypass.
After a gastric bypass, (and sometimes gastric sleeve), patients can encounter something known as Dumping Syndrome when eating foods high in simple carbohydrates such as sugar. For this reason, the bariatric diet does not include these foods.
Helpful Tips.
If you are getting uncomfortable when eating – for example, regurgitating, vomiting, or having a buildup of saliva after eating – this means you are usually eating too much or too fast. If you believe it is for none of these reasons, please contact the clinic so we can help you resolve any underlying issue that might be causing you problems.
-Try using smaller cutlery such as teaspoons rather than the usual knife and fork to help you to eat more slowly.
-When preparing specific bariatric diet recipes, don’t hesitate to halve the quantities to create a smaller meal.
-Serve your food on smaller plates and in smaller bowls to help to adjust to smaller portions.
-Do not drink anything too close to eating. Wait about 30 minutes after eating to start drinking again. It is important to remember that both food and drinks fill the space in your stomach and because you have had this stomach size reduced this it can be difficult to drink and eat at the same time.
-Avoid getting over-hungry as you are more likely to eat too quickly, leading to some discomfort.
Be in touch with your clinic if you need any further advise.
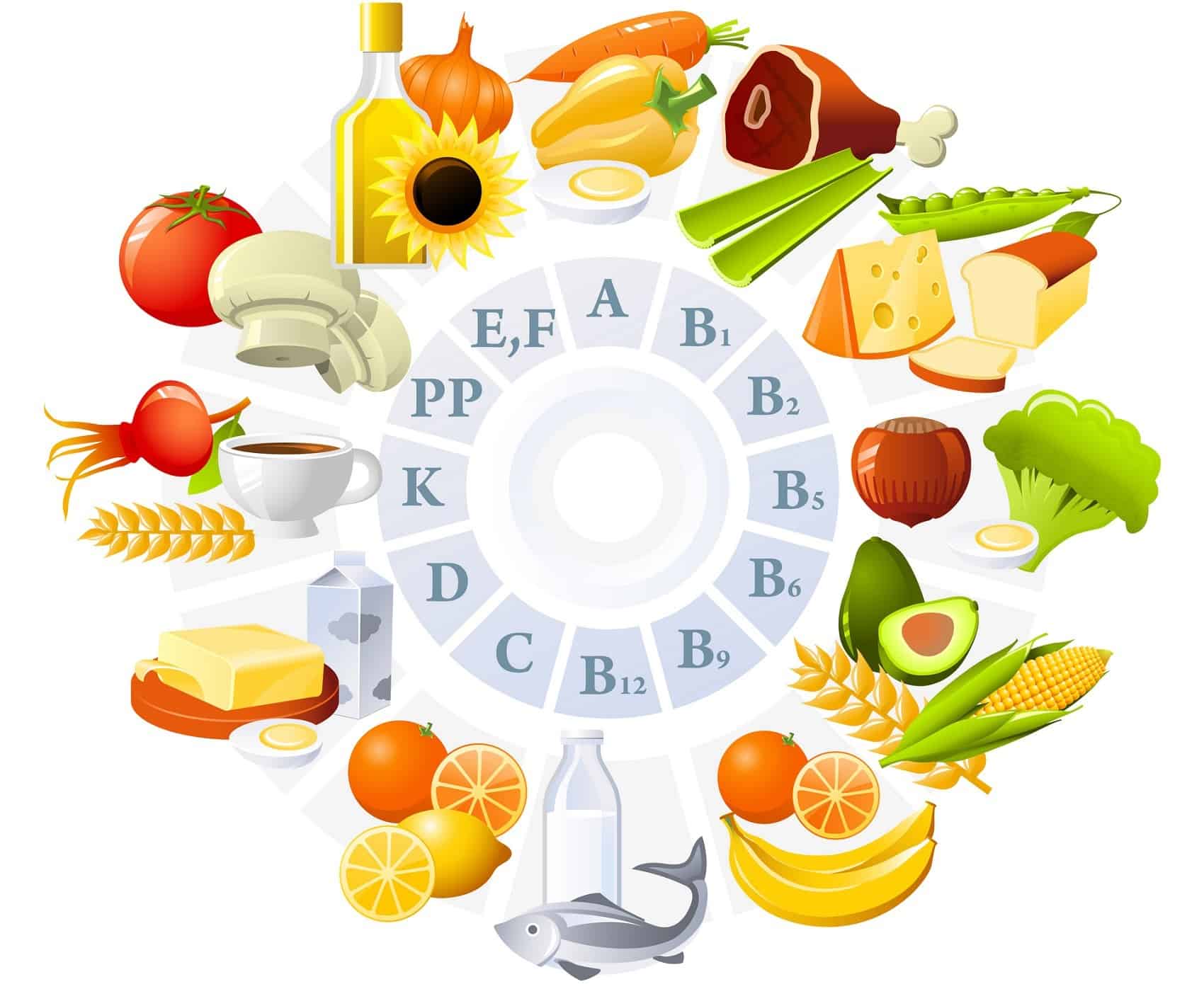
Vitamins and minerals
You will need to take a multivitamin for life.
You may need higher doses of certain vitamins or minerals, especially Iron, Calcium, and Vitamin D. You will also need to have at least yearly lab tests.
Learn More
Weight loss surgery can lead to reduced amounts of vitamins and minerals because people eat less and may absorb less in the intestines. Weight loss surgeries have different effects on vitamins and minerals based on how much change in absorption they cause. Deficiencies in vitamins, minerals, and protein can negatively affect health causing:
- fatigue (feeling tired)
- anemia (low levels of red blood cells that carry oxygen through your body)
- bone and muscle loss
- impaired night vision
- low immunity (your body’s ability to stay healthy)
- loss of nerve function (can affect your senses such as touch, taste, and smell)
- mental function deficits (changes how clearly you think)
Fortunately, nutrient deficiencies following surgery can be easily avoided with a good diet and the use of supplements including vitamins, minerals, and sometimes protein supplements. Before and after surgery, patients are advised of the appropriate diet and vitamin supplement needed. Most weight loss surgery programs also require patients to have their vitamins and minerals checked on a regular basis after surgery. Nutrient deficiencies and any associated health problems are preventable with monitoring and patients following diet and supplement (vitamin and mineral) recommendations. Health problems due to deficiencies usually occur in patients who do not regularly follow-up to monitor healthy vitamin and mineral levels. Be sure you stay in touch with your weight loss surgery team for best results!

Exercise and Lifestyle
-When can I start exercising after surgery?
-Will I have to exercise after the procedure?
Learn More
When can I start exercising after surgery?
Right away! To start, you will take easy, short walks while you are in the hospital. The key is to start slow. Listen to your body and your surgeon. If you lift weights or do sports, stay “low impact” for the first month.
Will I have to exercise after the procedure?
For many patients, exercise is important for stress control and appetite control, as well as burning off calories.
As we age, lack of activity can lead to being frail or fragile, which is quite dangerous to overall health. Healthy bones and avoiding muscle loss partly depends on doing weekly exercise.
Most patients also think of exercise as something that must be intense and painful (like “boot camp”). Regular, modest activity is far more useful in the long term. Even elite athletes can’t stay at a “peak” every week of the year. Instead, work with your surgeon’s program to find a variety of activities that can work for you. There is no “one-size-fits-all” plan. Expect to learn and change as you go!

Surgery to treat type 2 diabetes
Who is a Candidate for Diabetes Surgery?
A great deal of scientific evidence supports the use of diabetes surgery in patients with BMI of 30 and greater. If you have type 2 diabetes and a BMI of 30 and above, you may qualify for diabetes treatment through surgery.
View More
Surgery to treat type 2 diabetes!
Nearly all individuals who have surgery to treat diabetes (also called metabolic/bariatric surgery) show improvement in their diabetes, sometimes as quickly as a few days after surgery. They experience lower blood sugar levels, need less diabetes medications, and see an improvement in diabetes-related health problems. Overall, 78 percent of patients experience remission thus eliminating the need for diabetes medications.
Diabetes surgery performed today has been highly refined over the course of the past 70 years and is among the best studied therapies in modern medicine. These operations result in less food intake and decreased calories absorbed. Most importantly, however, these operations result in changes to the metabolism that affect intestinal hormones that regulate blood sugar control, often before the patient loses any weight. In addition, these procedures reduce hunger, increase the sense of fullness after meals, and assist the body’s ability to achieve a healthy weight. Diabetes surgery has been proven to be the most effective therapy for diabetes but also greatly improves obesity and other associated conditions.
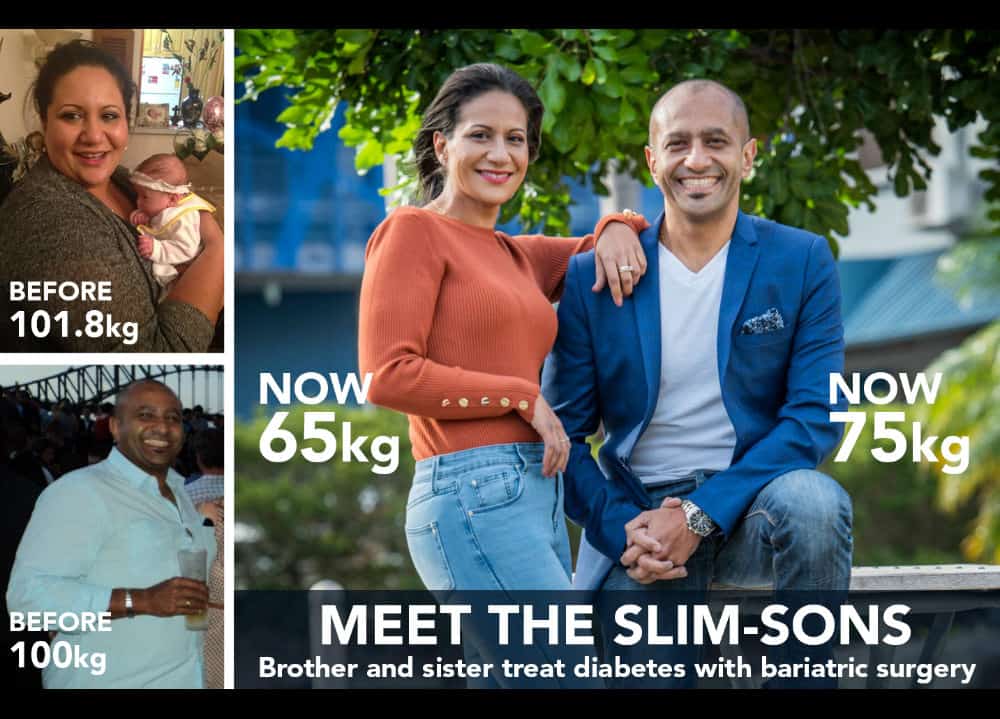
Bariatric Surgery for diabetes
Dr Jorgensen frequently treats multiple patients in the same family, with the same genetic predisposition to diabetes and obesity.
View More
This is otherwise known as “diabesity”.
An international coalition of 45 medical organisations recently agreed that surgery is now a standard treatment in patients with morbid obesity who are living with Type II diabetes.
This surgical pathway represents the biggest step forward in the treatment of diabetes in nearly 100 years. Find answers to the most asked questions on bariatric surgery for diabetes.
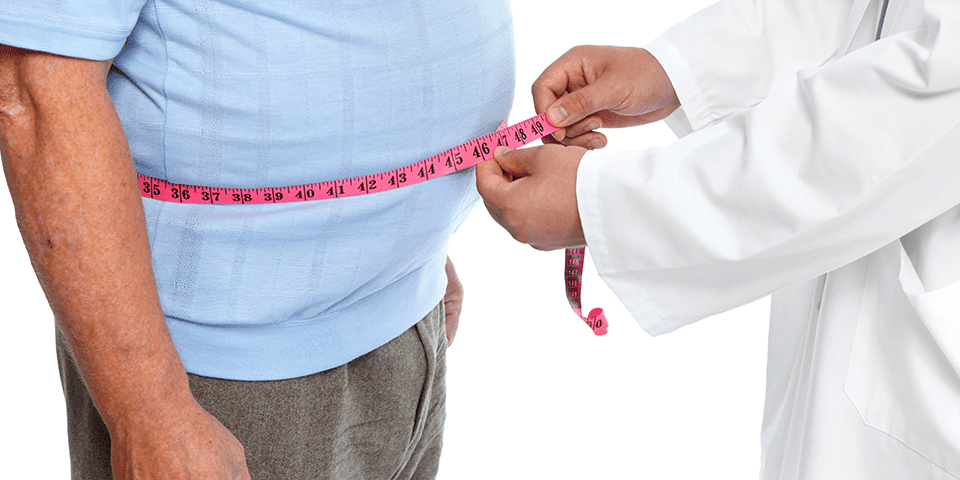
Defining Obesity and Measuring Obesity!
Obesity is no longer considered a cosmetic issue that is caused by overeating and a lack of self-control. The World Health Organization (W.H.O.), along with National and International medical and scientific societies, now recognize obesity as a chronic progressive disease resulting from multiple environmental and genetic factors.
View More
Defining Obesity
Obesity is no longer considered a cosmetic issue that is caused by overeating and a lack of self-control. The World Health Organization (W.H.O.), along with National and International medical and scientific societies, now recognize obesity as a chronic progressive disease resulting from multiple environmental and genetic factors.
The disease of obesity is extremely costly not only in terms of economics, but also in terms of individual and societal health, longevity, and psychological well-being. Due to its progressive nature, obesity requires life-long treatment and control.
Measuring Obesity!
The disease of obesity is characterized by an excessive accumulation of body fat. A variety of instruments are available for assessing the amount of fat versus lean tissue in the body. However, due to the expense of these instruments and the time required for body fat assessments, obesity is clinically defined by measures that ‘estimate’ adiposity from body weight, body build and height.
Ideal Body Weight (IBW)!
One of these estimates for body size is ideal body weight (IBW). The IBW table is based upon mortality data and requires knowledge of body weight as well as body frame, a measure that is considered by many experts to be arbitrary. Using this table, overweight and obesity are defined by percentage of weight in excess of IBW.
Body Mass Index (BMI)!
The body mass index (BMI) is another measure used to define overweight and obesity and is considered a more accurate estimate of body fatness than IBW. Large population studies find that the BMI generally reflects the amount of excessive body fat an adult has, although there are certain exceptions, such as the BMI of a woman who is pregnant, an athlete, a body builder or the elderly. BMI does not necessarily take into account a persons distribution of fat (abdominal vs. peripheral), however, and is not a good measurement of the metabolic activity of a person’s fat tissue.
BMI takes into consideration an individual’s height and weight can be determined by using a BMI chart or can be calculated according to one of the following formulas:
(1) Weight in kilograms divided by Height in meters squared (BMI = kg/m2)
Or
(2) Weight in pounds divided by Height in inches squared and this value multiplied by 705 (BMI= [(lbs/in2) x 705])
Body size categories using BMI have been based upon the ranges of BMI associated with a certain risk for mortality.
The categories and respective BMI categories are:
| Category | BMI Range |
| Normal Size | 18.9 to 24.9 |
| Overweight | 25 to 29.9 |
| Class I, Obesity | 30 to 34.9 |
| Class II, Serious Obesity | 35 to 39.9 |
| Class III, Severe Obesity | 40 and greater |
Weight Loss Surgeon Kogarah

Dr John Jorgensen is one of Australia’s most experienced Upper GI, General and Bariatric Surgeons.
He is Director of Bariatric Surgical Services at St George Private Hospital, Australia’s highest volume bariatric hospital and the first hospital in Australia to be recognised internationally as a Bariatric Centre of Excellence.
Dr Jorgensen recognises bariatric surgery as a new paradigm in the treatment of patients with Type II diabetes; with many patients either completely resolving their diabetes within days or weeks of surgery, or significantly reducing their medication.
